Alistair Fleming, healthcare expert at PA Consulting, argues that digitising surgery offers the potential to improve outcomes and enhance the reach of surgery
We’re on the cusp of a digital surgery revolution that will democratise access, drive efficiency and improve outcomes. Connected, patient-centric digital solutions are helping to address increasing pressures across much of the care continuum. However, surgery is still relatively data-poor.
Despite advances, surgeons still mostly rely on their own skill and judgement. Identifying which critical structures to avoid and diseased tissues to target requires years of training and experience but doesn’t guarantee outcomes. This skill barrier, coupled with aging populations, is creating a gap between the supply of, and demand for, surgeons.
Yet MedTech innovation could change this. Data-driven tools can help address skills shortages, improve outcomes and reduce cost.
Treat more patients by extending the reach and working life of surgeons
Surgeons are some of the most highly skilled and respected professionals, saving countless lives and improving the wellbeing of many more. But the need for such expertise means they’re in short supply. At the same time, skill and experience levels can vary, and the physical demands of the job can limit careers.
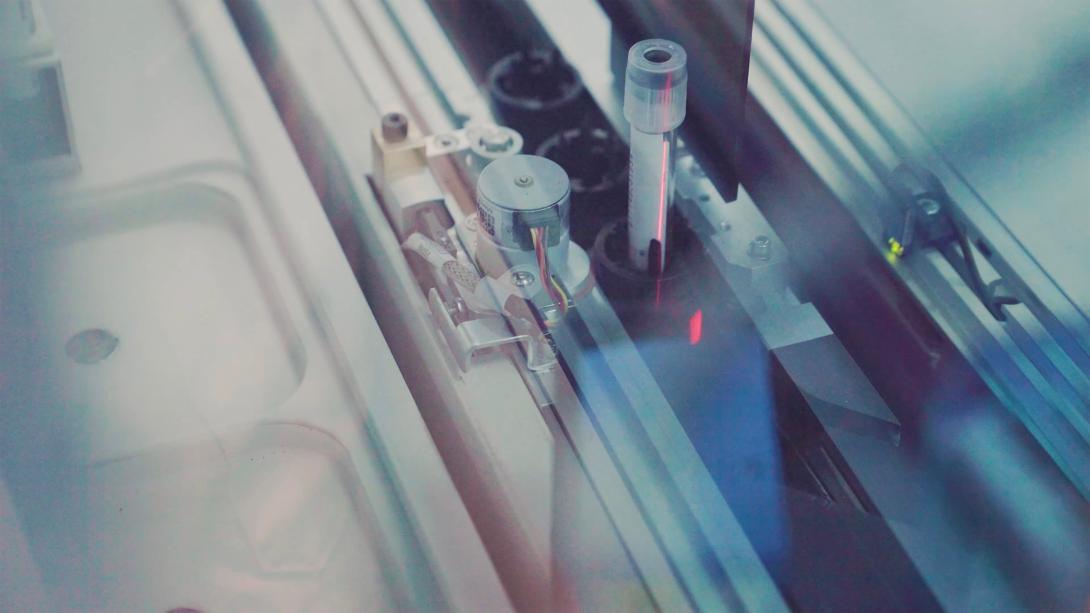
One way to help address these challenges is through Robotic-Assisted Surgery (RAS). Promising reduced fatigue, a steadier ‘hand’ and a shorter learning curve, RAS is already helping to extend surgeons’ careers and facilitate more consistent results.
RAS also offers the tantalising potential to extend not only the career but also the reach of surgeons, through remote operation. Historically, communication technology couldn’t offer the reliability and low latency remote surgery needs (in the order of 1-10ms), but 5G mobile networks and edge computing could. Indeed, isolated showcase surgeries have already been performed.
This opens intriguing possibilities. Research by the WHO has exposed massive disparities in access to surgery across the globe – on average, high income countries have more than 80x more specialist healthcare professionals per-capita than low-income countries. Densely populated areas also tend to be better served than rural communities. Telesurgery offers the potential for surgeons to deliver their skills into these underserved communities, despite being in a different part of the world.
Capitalising on the potential of 5G will require broad collaboration. The ITU (a specialised agency of the UN) helps to guide technical communications standards. They identified the ‘Tactile Internet’ as a concept embodying reliability and imperceptible time-lag, possibly using predictive AI, to enable remote haptic interactions, with application from healthcare to transport, education and culture. Since every link in the chain must support the requisite speed and robustness, RAS developers will need to engage with technology specialists, becoming systems integrator between hospitals, communications and cloud providers and regulators.
Optimise treatments though access to real time information
Robotic arms can make the job of operating easier, but the surgeon still needs to know what to target, how to get there and what to avoid, and technologies are coming to aid these decisions.
Already, pre-operative imaging is continuously improving diagnostics, enabling detailed planning, and this data is finding its way into the operating room (OR).
In orthopaedics and neurosurgery, intraoperative registration (overlaying scan data in real time) is relatively easy and has enabled solutions to guide, or even automate, aspects of surgery. But for most soft tissue procedures, registration is a much bigger challenge. Effective solutions in this space might require a mixture of pre-operative data and multi, or hyper-spectral, imaging, with the associated image processing and modelling. Hybrid ORs add the potential to incorporate other imaging such as CT and MRI, but these suites are costly and limited to larger institutions.
Aside from imaging, real time data acquisition can include signals from biomarkers, electrochemical responses, vitals and mechanical feedback. The objective with all these technologies is to help surgeons navigate their way to better outcomes.
Bringing this wealth of patient data and live feedback into the OR can also create challenges. Surgery requires intense focus, so information provision must meet three basic tenets: it must be timely, relevant and easily assimilated.
For example, solutions are appearing that use Augmented Reality to overlay visual feeds with imaging data, real-time feature identification and procedure metrics. These tools promise much, but innovators will need to engage clinicians throughout the development process to ensure the right balance of value to cognitive load.
Reduce the economic burden by personalising care and optimising resources
From genomic profiling to symptom tracking, the proliferation of digital health solutions is generating deeper insight that can steer treatment towards more precise care and more cost-effective approaches. This is just as relevant in the OR as it is in the wider care-continuum. Patient history can impact surgical events, and the outcomes of specific surgical interventions could drive bespoke rehabilitation plans.
To extract the most valuable insights and unlock the greatest benefits from digital surgery, datasets from diverse sources will need to combine. This presents some tough challenges. The security, (and public perception of the security) of patient data is paramount and has led to increasing regulation. Meanwhile, common data standards are yet to crystalise. As a result, data controllers and processors are grappling with how best to access and share information effectively.
From technology developer to provider, payer to government, and in the current rush for data, all stakeholders have a part to play in solving these challenges. We have seen that with clever use of anonymisation, population-level aggregation and consent-based access to patient data, new insights can drive more precise care without compromising patient privacy.
This requires collaboration and the onboarding of people with new skills and capabilities, such as data scientists, machine learning engineers and cyber and privacy experts. Obtaining such a range of new expertise might require partnerships with third parties.
The holy grail for surgery remains to be true intraoperative, patient-specific knowledge that guides surgeons to the best possible outcomes. Surgery offers infinitely more certainty than in its early days, but it’s still hugely challenging to navigate delicate vessels and nerves, to find malignancies and disease with pinpoint accuracy, and to precisely deliver the right intervention. Full integration and registration of patient data within surgery could finally give surgeons the information they need when they need it.
Digitising surgery offers the potential to improve outcomes, reduce costs, extend careers, enhance the reach of surgery, improve rehabilitation, aid training and lower the bar to proficient 21st century surgery. To realise this potential will require careful selection and deployment of leading-edge technologies alongside creative collaborations and a comprehensive appreciation of the unique complexities and pressures of the OR.